Don’t let it linger: Make these health appointments in your 40s and 50s
The biggest joke in my house is waking up and saying “oh, I guess _____ just hurts all the time now.” But we don’t have to live like this! Yes, it can be hard to get all your ducks in a row and go to a few doctors’ visits – even more so when you’re juggling career, home, kids, or just <gestures to world> life. But it’s your health, and you are important. If you’re in your 40s or 50s (and beyond), it’s prime time to make sure we’re living our best — and that means healthiest – “so-called” lives.
Starting at 40: get an annual mammogram
If you’re at high risk for breast cancer, you may need to start mammograms before 40. You can talk to your doctor about your risk level, but guidelines from the American Cancer Society note that:
“Women between 40 and 44 have the option to start screening with a mammogram every year. Women 45 to 54 should get mammograms every year. Women 55 and older can switch to a mammogram every other year, or they can choose to continue yearly mammograms.”
But it isn’t just about mammograms, really. It’s about understanding your risk, and your body. Have you ever done a self–breast exam? Or do you get an annual pelvic exam with a clinical breast exam by a doctor? Both of these can be helpful before you hit 40, but they’re not able to catch a potential issue as early as a mammogram or breast MRI can.
Who’s at high risk for breast cancer? Well, lots of women. But the American Cancer Society points out that those who should consider mammograms and other diagnostic tests at age 30 and older include those who:
- have a lifetime risk of breast cancer of about 20% to 25% or greater, according to risk assessment tools that are based mainly on family history (see below)
- have a known BRCA1 or BRCA2 gene mutation (based on having had genetic testing)
- have a first-degree relative (parent, brother, sister, or child) with a BRCA1 or BRCA2 gene mutation, and have not had genetic testing themselves
- had radiation therapy to the chest before they were 30 years old
- have Li-Fraumeni syndrome, Cowden syndrome, or Bannayan-Riley-Ruvalcaba syndrome, or have first-degree relatives with one of these syndromes
There are also guidelines for breast cancer screening for men and those who are transgender.

At 45, get a colonoscopy
I have secretly loved the last few years watching friends post on social media with the big gallon jug of laxatives and the comment IYKYK. Oh, I do.
As someone with Crohn’s disease, I’ve gotten colonoscopies since I was 29, when I was first diagnosed with the disease. The worst part, I tell friends, is the day of “prep” beforehand, when you can’t eat solid food, and have to pretend like you’re able to handle just some apple juice and black coffee for a day at work.
CBut colonoscopies are so important. And yes, you theoretically COULD “mail in your sample” with products like Cologuard, but if you’re at all at risk for colon cancer or other gastro diseases, or just want to get a good diagnostic look at your lower intestine, there’s nothing that’s as comprehensive as a colonoscopy. And at 45, you should get one. Just do it.
Don’t have a gynecologist? Why the heck not?
I can’t believe the number of women friends I have who don’t have a regular gynecologist. I don’t have kids, but I still like to get regular pelvic exams and make sure things are good under the hood (so to speak).
The good news is, you don’t need a full OBGYN doc to get annual exams or pap smears. Medical professionals like nurse practitioners, physician assistants, or midwife nurses can also perform these tests, and they can be a lot easier to schedule with than in-demand docs. Early detection can be so key through these exams.
Remember, too, that a pelvic exam can help diagnose a lot of issues you might be concerned with, but don’t usually associate with your reproductive system (or at least, not at first). For example, the Mayo Clinic lists the following as conditions treated in their OBGYN department:
- Abnormal Pap smear
- Abnormal or heavy uterine bleeding
- Cancer
- Endometriosis
- Heavy menstrual bleeding
- Hot flashes
- Infertility
- Menopause
- Ovarian cysts
- Pain during intercourse (dyspareunia)
- Pain during periods (dysmenorrhea)
- Pelvic organ prolapse
- Pelvic pain
- Postmenopausal bleeding
- Premenstrual syndrome (PMS)
- Sexually transmitted diseases/infections
- Urinary incontinence
- Uterine fibroids
- Vaginitis
- Vulvodynia
You might notice a few, like hot flashes, urinary incontinence, and clearly menopause and postmenopausal bleeding, that can all fall under the category of things you might start dealing with in your 40s. You can also get bloodwork or testing done to check for sexually transmitted diseases or infections or get an IUD inserted or removed at your OBGYN.
Think you’re due for a pap smear? You might get to hold off if you’re low-risk and over 30. The current guidelines don’t require yearly pap smears for women “of a certain age” like us Gen Xers and elder Millennials.
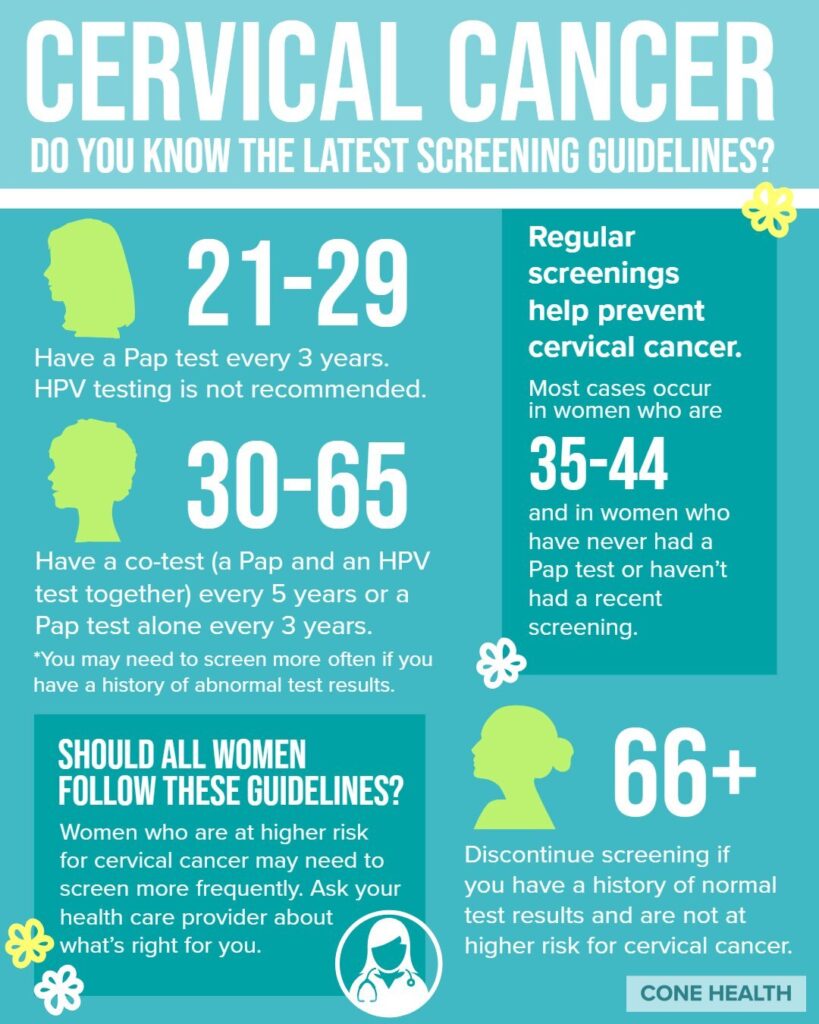
According to the American College of Obstetrics and Gynecologists (ACOG):
- Women ages 21 to 29 should have a Pap test alone every three years. HPV testing alone can be considered for women who are 25 to 29, but Pap tests are preferred.
- Women ages 30 to 65 have three options for testing. They can have both a Pap test and an HPV test every 5 years. They can have a Pap test alone every three years. Or they can have HPV testing alone every five years.
- After 65, you can stop having cervical cancer screenings if you have never had abnormal cervical cells or cervical cancer, and you’ve had two or three negative screening tests in a row, depending on the type of test.
This doesn’t mean you should avoid a GYN forever, though! You should still see a doc and get checked every single year. And if you’re trying to figure out treatment for menopause symptoms through prescriptions like hormone-replacement therapy, you’ll want one that you can talk to regularly about how you’re feeling, what’s working, and what isn’t.
Get your moles checked — and find a good dermatologist
Get a dermatologist for mole checks and skin-related aging questions like how to deal with stretch marks, spider veins, and weird hairs. Mine helped me deal with perimenopausal hair loss AND discovered that I have low-iron anemia! You can also see a dermatologist for all those fancy skin treatments like lasers, Botox, and fancy face peels. Those come more with private practice derms, rather than ones at hospitals or major medical centers, but both have their place.
Tip: Be prepared to schedule a few months out for your dermatology appointments. They’re high in demand for everything from weird, sudden rashes to long-term skin problems like eczema or psoriasis or even skin cancer.
Get a physical therapist for your pelvic floor (and stop peeing when you sneeze!)
Physical therapy isn’t just for busted-up shoulders or when your foot gets fractured during a 16-inch softball game that you played while half in the bag (I see you, beer league). You might start looking for a pelvic floor PT if you’ve recently had a baby or if you’re just tired of wearing that panty liner and crossing your legs when you feel a cough coming on. But it can be hard to figure out what department of a medical center they operate out of.
Due to bad website keywords and a wimpy search function, I had an impossible time finding one at my own local hospital until I realized they weren’t under “urology” or “OBGYN” For me, the docs I wanted were still in the physical therapy department but were nestled under Occupational Therapy, which includes finding help doing physical things after a major injury. You might see OT if you have a bone fracture from a fall, for example, and need help figuring out how to use a wheelchair or shower stool at home. But you should see a “Pelvic Health Rehab” specialist or “Pelvic Floor” specialist if you want to stop peeing on accident.
Don’t be ashamed! Women can experience changes in the strength of their pelvic floor when their hormones change during menopause or perimenopause. And it also can be a great first step to see if PT and home exercises are the right fix for your problem, or if something like surgery could help!
Get a therapist you like!
Look, most of us don’t have a problem with getting therapy, but lots of us struggle to find that therapist who we truly vibe with. Or we don’t know how to find one that our health insurance might help pay for. First thing’s first, if you have besties who see a great therapist then ask them about why they like going to them. Maybe they feel like someone is finally listening to them for the first time in their lives. Or they have someone who they feel is of a similar age or background. Personal referrals are always a bit more candid than that dreaded “personal bio” doctors now write about their practice along with their “personal philosophies.” If that therapist isn’t taking on new clients, you can always ask them to offer up a few folks that THEY like. It can help you cut down on the “first dates” and get right to the healing.
Find therapists in your area without thumbing through a Google search with online directories like this one from Psychology Today. You can see details about them, read their credentials, and see if they’re taking on new patients. You can also see what kinds of specialties they have, and check out what insurance they take (not always a complete list, so definitely ask your insurance if the doctor is in-network or not). Call your insurance “customer service” line to check your in-network requirements and what kind of mental health services they cover. You might be surprised.
Don’t have health insurance? Check to see if you can get a plan through the Affordable Care Act. Most of these tests, if not all, are not mandated to be 100% covered by all health insurance plans thanks to the ACA. (Thanks, Obama!)




