My $3,000 journey to self-diagnosing perimenopause
General and sustained shittiness. It was difficult to articulate exactly what I was experiencing, as my symptoms were numerous. I’d been on the hamster wheel for five years — juggling motherhood and a demanding career in tech marketing. As a former athlete, I knew what it was like to feel strong in my body and mind. This was not it.
Was I feeling terrible because I hadn’t gotten quality sleep in years? Was it the increased work stress? Were the compounding effects of raising young kids during a pandemic (and that late-night doom scrolling) finally catching up? After months of knowing I wasn’t in a good place, I decided to make health my No. 1 priority. This is where that journey took me.
The maddening state of midlife healthcare for women
At 38, I saw a neurologist for chronic headaches, an acupuncturist on the recommendation of a friend for bloating, cramps, and generally not feeling well. I went to my OBGYN, saw a therapist, tried The MyFLO app, started taking supplements, and more. The winding path was inefficient, expensive, and extremely frustrating.
If it feels like you’ve suddenly reached the limit of what your primary care doctor or OB/GYN can provide, you might have arrived at what I’m calling the “midlife care cliff.” It’s the point where most women will benefit greatly from seeing someone who specializes in hormone health and treating hormone-related symptoms. Unfortunately, most of us fall into one or all of these groups:
- We don’t recognize that our various symptoms could be hormone-related.
- We don’t know where to find clinicians who are hormone health specialists.
- We have been dismissed or unintentionally misled by doctors who aren’t knowledgeable in hormone health or the menopause transition themselves.
- We have run out of time, money, or energy to keep seeking help.
Ideally, we would all seamlessly graduate to a “MENO/GYN” except that isn’t really a thing (at least not yet).
The absurdly high cost of getting a perimenopause diagnosis
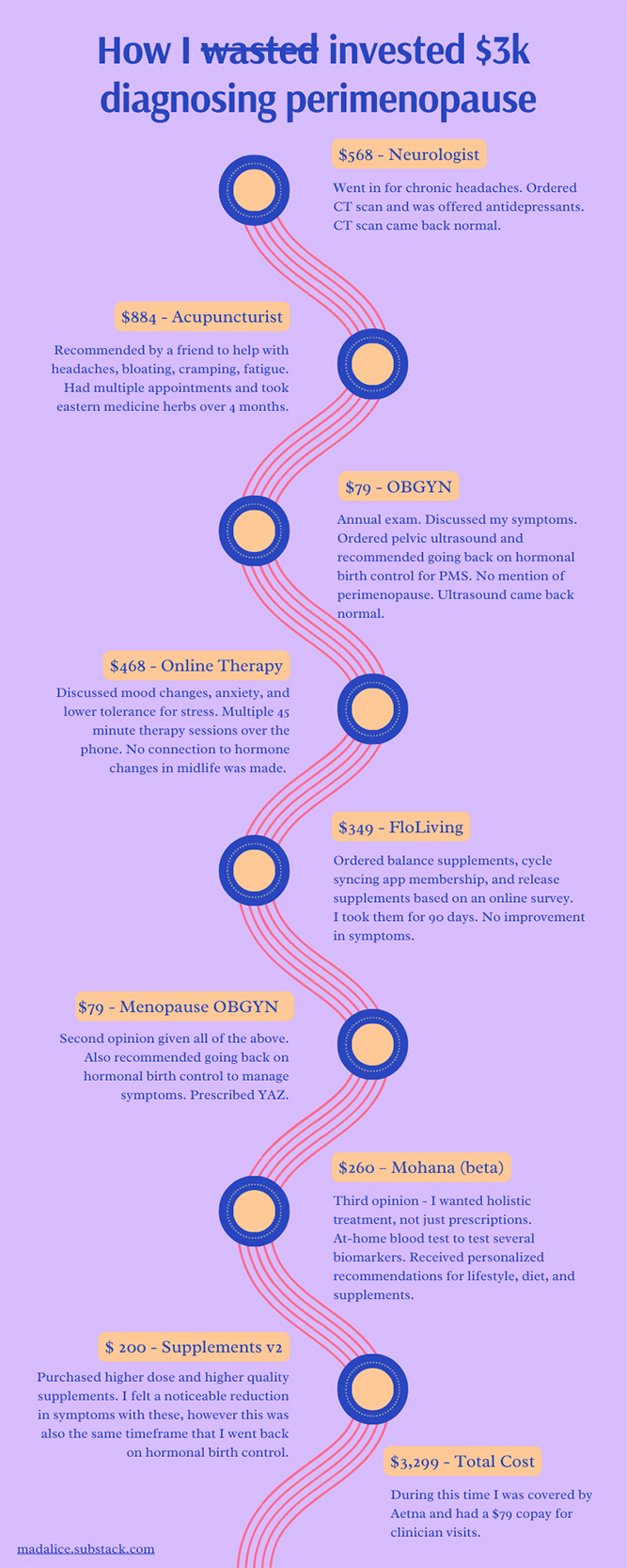
Eventually I pieced together a care plan that returned sustained positive results. My formula included going back on hormonal birth control to reduce PMS symptoms and incorporating very specific supplements, diet, and lifestyle changes to reduce inflammation, thanks to my Mohana care plan. Treating my common perimenopause symptoms should not have taken this long, been this expensive, or required so much research. But here we are. This is the state of women’s healthcare in 2024.
What good care from perimenopause-trained doctors should look like
In my opinion, it’s ridiculous that I had to do hours of research online, spend more than $3,000, and see six providers to get to a care plan I started seeing good results with. Women do not have the resources to do this.

This is what adequate care from perimenopause-educated clinicians could have looked like in my journey:
- The neurologist could have asked what other symptoms I was experiencing and pattern-matched them with perimenopause given my age (over 35). I could have been referred to a hormone health specialist before we went ahead with the CT scan or the prescription for antidepressants to help with headaches. A patient intake form could also have been optimized to help here given my age and sex given that headaches are a very common symptom during the menopause transition.
- The acupuncturist (who specializes in women and reproductive issues) could have mentioned that I might be in the early stages of perimenopause. They could have offered that many women feel better going back on hormones, and what the other options were for treatments in addition to acupuncture (which has limited clinical evidence).
- My OBGYN could have offered blood tests to measure my metabolic, vitamin, and hormone levels before recommending going back on birth control. They have given me a pamphlet or other information on perimenopause or even mentioned that word to me. They could have pointed me at some of the great resources from experts in this field (looking at you Dr. Mary Claire Haver!). I was handed an entire book and educated about various apps I could use after confirming my first pregnancy at six weeks — where is the proactive education for the menopause transition?
We have got to do better for women.
People born with ovaries who are 35+ years old represent more than 25% of our population. And 85% of us will have adverse symptoms during the long transition to menopause.
How to find a hormone health specialist for perimenopause
I want women to stay in the game. And personally, I want to have a FANTASTIC second half. Over time, I’ve come to accept that being born with the bits to create human life comes at a cost, but it shouldn’t be this high.
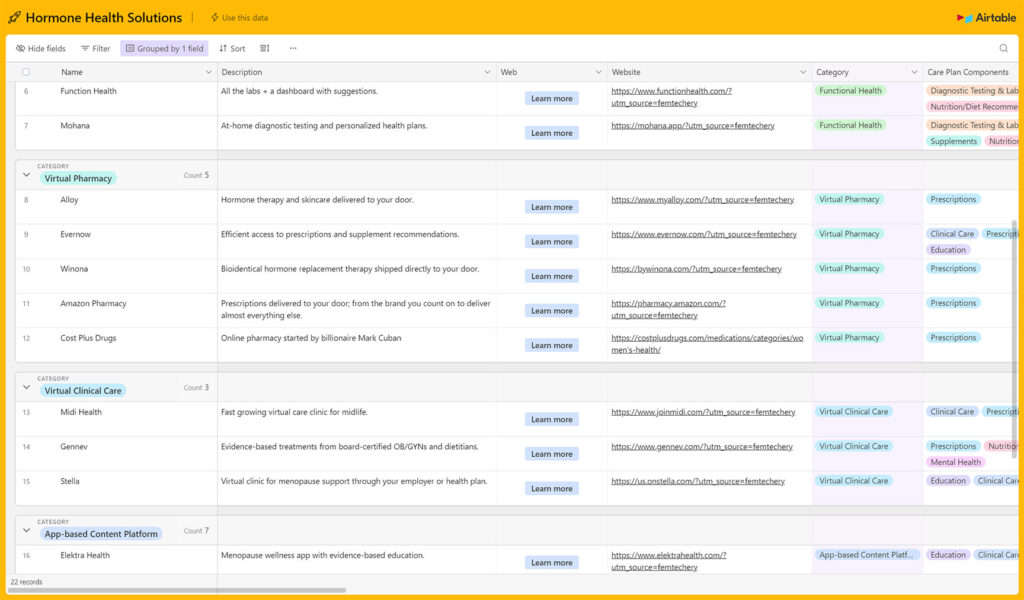
In an effort to help more women efficiently navigate the ecosystem of offers in this space, I created a menopause specialists database. It includes a scannable summary of platforms and providers for women in the menopause transition. Many of these providers also have excellent solutions for managing PCOS, endometriosis and other hormone health concerns.
Imagine how we will change the world when every person born with ovaries feels full of energy, free of pain, physically strong, and cognitively sharp. THAT is the world I want to live in.
This article was originally published here on Mad Alice.