“Healthy tan” then, skin cancer now
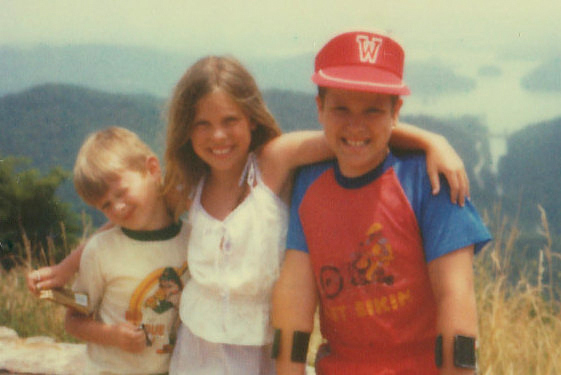
Many of my childhood memories involve things that probably weren’t the safest. Riding up-front between my parents on long car trips. Inhaling smoky, nicotine-filled air that blended into the orangey-brown earth-toned décor and wallpaper. Drinking bright red Kool-Aid and eating Crisco cookie dough. Doing penny flips off the high monkey bars over a layer of jagged rocks. Biking or walking wherever I wanted without anyone knowing where I was. And my favorite activity of all: spending summers at the pool with no sunscreen, hats, or cover-ups.
In our suburban Chicago town, a summer pool pass was an affordable luxury for our family of six. An escape from our un-airconditioned two-bedroom townhome. My mom could have a desperately needed rest at the poolside, before working the night shift. My brother Teddy, who has spina bifida, could have a break from his crutches, able to swim as well as anyone and even dive off the diving board.
Sure, I learned to swim — though my husband might challenge me on that statement — but I mostly loved jumping around in the water with lots of great ’80s music playing in the background. In 1983, our pool’s straight, metal slide was replaced with a pair of twisty plastic water slides called “The Daredevil” and “The Pipeline.” Should I choose the better slide with the longer line? Always a hard choice.
I learned lots of things while being in a pool with a wide swath of people. I learned that being Dexatrim thin like a Barbie doll was almost possible. I learned that hair can grow in odd places. I learned that some kids were really mean. I learned that once girls became teenagers, their appearance became everyone’s business. And a belly flop off a high dive taught me all about kinetic energy (painfully).
When my mom started working during the day, she often dropped my brothers and me off at the pool during her lunch hour and picked us up after work. We’d bring our swimsuits, maybe some towels, a dollar or two for nachos or ice cream, and that’d be it. And I loved it. Each summer, my skin color gradually deepened into a golden shade, only noticeable by the tan lines that faded each fall.
I wasn’t trying to look like my Malibu Barbie, but I did like the complements I’d get on my “healthy” tan. When I showed up each August for my annual check-up, even my pediatrician approved. I once asked her about a small birthmark on my thigh, hoping she had some magic medicine to make it disappear. Instead, her board-certified advice was, “just get some sun and no one will notice.”
During the ’90s, I headed indoors and began avoiding pools, keeping my natural Fitzpatrick skin type 2 year round. Not because I was worried about UV radiation, made worse by the thinned ozone layer, but more because I felt self-conscious of my (in reality very average) weight.
As a teenager, I no longer felt comfortable in a swimsuit. Despite drinking milk every day, I definitely didn’t grow more confident with my body as I grew older, as I was promised in the “Milk…It Does a Body Good!” ads. So maybe my “thunder thighs” (as judged by pre-2000s beauty standards) spared my skin from further damage, because I’m pretty sure that if I had a Beverly Hills, 90210 body then, I’d have racked up even more UV radiation during the Britney-bronze decade.
Once I entered my thirties, I began going to regular skin screenings, knowing that at some point I’d likely get a skin cancer diagnosis based on my early life sun exposure and fair skin.
My BCC skin cancer diagnosis
Two months ago, it happened. A few millimeter basal cell carcinoma (BCC) was removed from my nose. I’m glad I had my skin looked at by a dermatologist, because the small, skin-colored bump looked pretty similar to other benign skin imperfections that often begin showing up on faces of people my age.
BCC is the most common form of skin cancer, and the most common type of cancer in the world. While it’s the least risky type, it can be disfiguring if not caught early. The sooner, the better: seemingly small skin cancers can sometimes be a “tip of the iceberg,” where the cancer spreads out below the surface.
Once the diagnosis of skin cancer is confirmed, further treatment is usually needed, and in most cases, a surgical removal of additional skin tissue is done to ensure “clear margins,” the complete removal of cancerous cells in the area. If the cancer is located in a sensitive area of the body, such as the face, a procedure called Mohs surgery is typically performed, because it preserves as much of the healthy skin as possible.
A few weeks ago, I underwent this outpatient surgery. Thankfully, clear margins were obtained after the first layer of skin was removed (oftentimes multiple excisions are needed). I ended up with a 2 centimeter line of stitches (covered with Steri-strips) smack dab in the middle of my face. The stitches came out last week and the Steri-strips just came off. Healing usually takes six to eight weeks, but the redness, the nurse told me, will be the last thing to go.
When the healing process ends, a noticeable scar will almost certainly be left. But I’ll gladly take the scar, because if the cancer was left in place, it would have been much worse. I’m also aware that this personal history of skin cancer puts me at higher risk for another. But I’m not going to worry (too much), because the bottom line is: skin cancer is preventable and 99% curable when caught early.
To help parse out how past sun exposure can affect our risk for skin cancer today, I talked to board-certified dermatologist Dr. Mark Allan Berk, MD FRCPC, founder of The Skin Care Center (with offices in Chicago, and north suburban Glenview and Lake Forest, Illinois) about how to think about our sun history and personal risk factors. and more importantly, what we can do now to protect our skin going forward.
Dr. Berk’s best “in a nutshell” skin-cancer prevention tips
Daphne Berryhill: When I told my mom I had skin cancer, she was surprised because I’ve been so sun-safe as an adult. Can you explain to our readers why early life sun exposure has such significance years later in terms of skin cancer risk?
Dr. Mark Allan Berk, MD FRCPC and founder of the Skin Care Center: Sun damage is cumulative, and younger people are sometimes less likely to be sun-safe!
I have a basal cell at 47. My sister-in-law was diagnosed with an early stage melanoma just before 40. I know other women in early midlife getting skin cancer diagnoses too, without having significant tanning or family histories. I don’t see that same pattern within older generations of my family, even though they didn’t wear sunscreen. Are you seeing this trend on a larger scale in your clinic and if so, do we understand why?
In my practice it is really clear that two patients with very similar skin and sun exposure history, can have totally different experiences with skin cancer, because genetics have a major effect. And melanoma and basal cell are very different. Some say up to 50% of melanomas are not directly related to sun [exposure]. But basal cells are almost always sun related!
Are regular skin screenings needed for everyone?
Everyone should do a monthly skin self-exam and have a total skin exam yearly.
Is sunscreen really needed every day, even for people with darker skin tones? Are there any specific active ingredients in sunscreen products that you recommend over others, or is anything with an SPF of at least 30 sufficient for daily usage?
Since we can’t always predict if we might need to be outside, sunscreen is recommended daily for everyone. Zinc Oxide and Titanium Dioxide are the best ingredients that we have here in the U.S. and should be used at SPF 15 to 30. Those of us with more natural pigment might use products with less, such as SPF 15.
If we’re not seeing our skin color change after we’ve had sun exposure, can we assume that our skin was adequately protected?
No, most sun damage accumulates over many years even with very slow tanning of the skin. Severe damage occurs with sun burns. But I always advise that our skin never forgets and never forgives.
So in general, the lighter your skin, the greater the risk from sun exposure. But, it’s also true that anyone can get skin cancer, and people of color are often diagnosed in later stages. What skin precautions do you recommend for POC?
People of color and even their doctors often don’t realize that POC do get skin cancers, so unfortunately their skin cancers may not be noticed until the later stages. The same skin checks I mentioned before, with a particular careful examination of the palms and soles, are recommended for early detection and sunscreen for the prevention of sun damage.
I work in a cancer center where we occasionally treat patients with skin cancers that have spread. While there are game-changing therapies available today, catching them in earlier stages where surgical removal is the only treatment needed is much better, and sometimes life-saving. Do you have any recommendations for catching skin cancers that often get missed in the early, more treatable phases?
Good skin examination with help from their dermatologist is the best along with sun protection. If theirs is a family history of any skin cancers, the [annual] skin exam is especially important. There are new exciting diagnostic tools that are being developed for the early diagnosis of skin cancer but not available for home use yet.
Can you recommend any websites that provide reliable skin cancer information, including pictures of what to look for in a range of skin tones? Are there any skin-screening apps you recommend to your patients?
Of all the apps and websites, the best source of info has been and remains the American Academy of Dermatology website AAD.org.
While there’s growing awareness about the dangers of UV exposure from the sun, we’re also understanding how important sunlight exposure is for vitamin D production, mood and sleep. How should we think about balancing these benefits with the risks?
The sun is so good for us but it is bad for the skin. It causes skin cancer, wrinkles, and more — a real paradox. I can’t truthfully recommend an amount of sun exposure that is safe and that will provide enough Vitamin D without causing cumulative sun damage. So, I recommend natural healthy sources of vitamin D that are easily available either in our diet or as an oral supplement.
Sorry, the comment form is closed at this time.





Vivian Schroeder
Such great advice!
Lucia Kanter St Amour
Daphne, thanks for sharing your story. My friends and I used to sun bathe with baby oil as a teenager – insanity!! And, per your bio, your observation is so apt that “something sucks about being every age.” Though I wouldn’t go backwards to any age (at least not yet)!