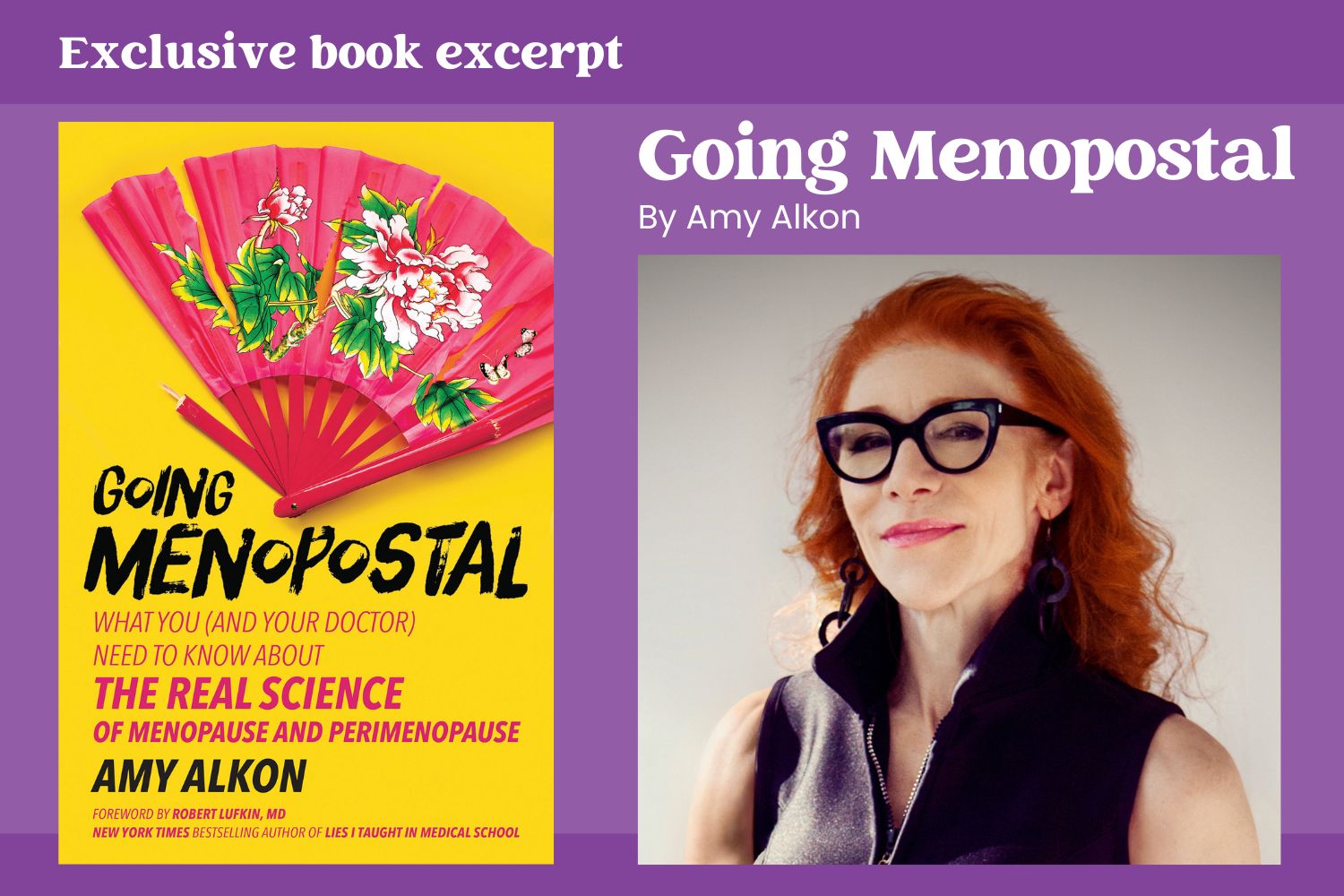
Are you Going Menopostal? Amy Alkon digs into what you really need to know
This is an exclusive excerpt of Going Menopostal. Reproduced with permission from author Amy Alkon (BenBella Books, 2025).
THE EMPEROR’S NEW LAB COAT: Calling out the bad science behind medical practice standards for menopause and perimenopause
In 2016, when I had that first hot flash and began my dive into research on menopause and perimenopause, I noted a disturbing parallel with the saturated fat debacle: researchers clinging to scientifically unwarranted beliefs about menopause and perimenopause—dismissing any pesky evidence that called their beliefs into question.
Doctors, reasonably, don’t think to question the scientific basis of the research behind the menopausal and perimenopausal practice standards their department requires them to go by. (Who would imagine a respected medical institution’s treatment requirements would have anything but a solid scientific foundation?)
I, however, was able to see the often-unscientific underpinnings of menopausal and perimenopausal research and medical care—not because I’m some sort of genius, but because I’m a medical outsider, coming in largely cold to the subject matter.
I approach medical science taking nothing for granted—including the foundational beliefs in a field: those “facts” everybody in the field “just knows” (like all those gastroenterologists “just knowing” ulcers were the fault of the patient for having that stressfest of a job and marital problems, too). I look not just at current studies but dig into medical history, starting with the first findings in the field and working my way up to the latest research and thinking.
Still, I was cowed by what a huge and truly terrible responsibility writing and publishing this book would be. If I’m in my usual neighborhood, behavioral science, and I do a bad job assessing the research, somebody might say the wrong thing to their boyfriend and kill their relationship. If I get medical science wrong, somebody could be harmed or maybe even die. I struggled with what to do, and then it occurred to me: In writing this book, I wouldn’t be without a scientific net. I would do what I do with every science-based book I write: send chapters and sections out for fact-checking by experts in each area—researchers whose scientific rigor I respect—and beg them to “hand me my ass” in any places I might’ve erred or fallen short.
Ultimately, I wrote this book because I couldn’t live with not writing it.
No, I don’t wear a white coat, and the last time I held a stethoscope, it was plastic and I was six. What I do have to offer you are the benefits of my drilling down in the research to find the most powerful, efficient ways for us to stay strong and healthy throughout our lives. You deserve what I was able to get for myself—evidence-based care to ease the life-chomping symptoms of menopause and perimenopause. You deserve to join me in flipping the bird to the inevitability of ill health in old age.
WHAT IS PERIMENOPAUSE?
“Peri” is the ancient Greek word for “around,” so perimenopause is the time around menopause—basically the on-ramp to menopause. It can start as early as a woman’s mid-30s and can last from three to 10 years (or more in some women) and ends when a woman goes into menopause.
What marks the start of perimenopause? Well, there’s the standard, widely accepted but physiologically incomplete view—leaving out women just starting perimenopause and feeling newly crap-o-ramous—and then there’s the more physiologically precise view that reflects what those women actually go through, hormonally and symptomatically.
The standard view is myopically menstrual cycle–focused, and it comes from a collaboration of researchers called STRAW, the “Stages of Reproductive Aging Workshop.”
The STRAW panel announced that perimenopause starts when women begin having persistently irregular menstrual cycles—or as they call them, “variable.” “Variable” means that the number of days one menstrual cycle lasts varies from the length of the next by seven or more days. “Persistently” means this fluctuating-length thing repeats itself (at least once within a span of 10 cycles). For example, in May, a woman’s period comes just 28 days after her previous one, but in August, she gets her period only 20 days after the one in July.
Now, STRAW’s description of irregular menstrual cycles isn’t wrong. And healthy women with regular menstrual cycles do eventually experience irregular cycles in perimenopause. But STRAW’s claim—that ONLY upon menstrual cycles getting irregular is a woman in perimenopause—fails to take into account the hormonal changes occurring before cycles get irregular, documented by gynecologist Nanette Santoro, Dr. Prior, and other researchers.
These early hormonal changes ignored by the STRAW team trigger a set of symptoms (detailed below) in still-regularly-menstruating women that should lead doctors to diagnose the start of perimenopause (and determine the appropriate treatment, if necessary). However, because STRAW ignores the inconvenient evidence that conflicts with their foregone conclusions on timing, and because STRAW is baked into practice standards, the perimenopausal symptoms these changes trigger are a medical no-man’s-land—not traceable to any particular cause.
Diagnosis: Inexplicable medical mystery! (Just the thing for emotional tranquility when yoga, meditation, and maniacally raking the sand in your desktop Zen garden aren’t doing the job!)
NINE CLUES YOU ARE IN PERIMENOPAUSE
Figuring out whether you’re in perimenopause—diagnosing yourself so you can get your symptoms treated appropriately—doesn’t take years of med school, a slew of blood tests, or a mini MRI in your she-shed.
In fact, you probably mastered the special diagnostic skill this requires some years back—in nursery school, when you learned to count. That’s really all it takes. You skim a quick list of perimenopause symptoms, tally up how many you’re experiencing, and see whether you hit three.
Detecting whether you’re in perimenopause does take a lab, but that lab is you. The earliest perimenopause symptoms are mostly forms of menstrual cycle suck gone much suckier: the result of a brewing storm of hormonal unrest in you in the earliest days of perimenopause.
The very simple task at hand? Going through that “quick list” I mentioned and counting up the number of symptoms you’re experiencing that make you feel like you need an exorcism instead of an Advil.
Endocrinologist Jerilynn Prior, MD, puts it more technically: “Perimenopause begins with changes in experience” in your body and brain as a woman in your “midlife” years. (Midlife starts around age 40, though there are women who go into perimenopause in their 30s—or in their 50s.)
Take swollen boobs—no stranger to any woman who’s ever shopped the period products aisle. Before perimenopause, it’s normal for the breasts to swell during the weeks before flow, Prior explains. The changes pointing to perimenopause? Your boobs see no reason to limit this swelling business to PMS time. They might even be swollen most of the time—and much more swollen and sore than you’re used to. (For a while in perimenopause, I had to sleep in a bra so I wouldn’t wake myself screaming when I rolled on my side and had boob-to-sheet contact.)
Prior and her colleagues came up with this list of changes you can use to self-diagnose perimenopause. You’re in what Prior terms “Very Early Perimenopause” if you still have regular menstrual cycles about a month apart, yet experience any three of the following:
- New onset of heavier and/or longer menstrual flow.
- Shorter menstrual cycle lengths (25 or fewer days between periods).
- Breasts that are newly more sore, swollen, and/or lumpy.
- New or markedly increased menstrual cramps.
- Waking up mid sleep when this was not previously an issue.
- New onset of night sweats, especially around menstrual flow.
- New or much more frequent migraine headaches.
- New or more frequent premenstrual mood swings.
- Notable weight gain without changes in food intake or exercise habits.
These symptoms can hang around bothering you for several years before there’s any change in your menstrual cycle (from regular to irregular), notes Prior. Unfortunately, your medical institution most likely doesn’t use this symptom-checking method for diagnosing the early stages of perimenopause—not because it’s inaccurate, but because it’s standard practice in the field to go by that timetable the STRAW (Stages of Reproductive Aging Workshop) panel came up with.
The STRAW guidelines underestimate the actual length of perimenopause (suggesting it lasts only two to four years). They come up short due to the STRAW team’s physiologically unsupported claim that only when women start experiencing irregular menstrual cycles—seesawing in length from one to the next by seven or more days—are they in perimenopause.
Because women often get hit with the hormonal and symptomatic unrest of perimenopause while they still have regular periods, the STRAW standard that excludes their experience sticks them with looming uncertainty about what might be wrong with them.
Uncertainty—provoking fear of the unknown and what it might hold—is deeply disturbing to us, causing uncomfortable psychological tension. Some women become driven—even desperate—to alleviate it, seeking out what Prior describes as “(disease) diagnoses,” such as fibromyalgia and chronic fatigue syndrome, to “explain and legitimize” their suffering. This may cause them to get treatments they don’t need that sometimes cause lasting damage.
The damage can also be psychological, Prior explains. To manage the looming uncertainty about the cause of the symptoms, “A perimenopausal woman may start viewing herself as chronically ill.” That’s a term for feeling persistently sick, which is very much how I felt in perimenopause—though it’s a bit institutionally beige to convey my constant undertone of panic at suddenly feeling so swollen, weak, broken-down, and old.
HOW LONG MIGHT THIS PERIMENOPAUSAL HELLSHOW LAST?
It’s important that you know when you’ve hit perimenopause and where you might be in the progression to menopause, both so you can tell your doctor in hopes of getting appropriate treatment and so you have an idea of what to expect.
Dr. Prior and her colleagues created a physiologically accurate map of the stages leading to and through perimenopause and menopause—a timeline that, vitally, includes the “Very Early Perimenopause” phase STRAW left out, when women with still-regular menstrual cycles start suffering uncomfortable changes.
This led Prior and her team to conclude that perimenopause typically “lasts several years and commonly lasts six or seven.” That said, women’s experiences vary widely, and a number of us have a much shorter or much longer stint in perimenopause. (Mine was basically a perimenopausal decade.)
Accordingly, the Prior team’s stages of menopause and perimenopause below are not a template your experiences should conform to but a general idea of how things might play out for you.
Very Early Perimenopause:
The stage you’re likely in if you check off three or more symptoms on Prior’s nine-item list (“The Nine Changes” above). “This phase may last from two to five years,” writes Prior, and “probably lasts longer in those who start it in their 30s” than in those getting started on these changes in their 50s. (Which, yes, happens!)
Early Perimenopause (aka the “Early Menopause Transition”):
“The onset of irregular cycles (varying by 7 days from the start of one flow to the next)” heralds the beginning of this stage, explains Prior.
Late Menopause Transition (taking place in perimenopause):
“The landmark of the first skipped period” on the road to menopause, writes Prior.
Very Late Perimenopause:
“The last count-down year” to menopause, writes Prior—or, in lingerie terms, the year after your last period ruins its last pair of cute underpants. After 12 months straight without flow, you’re in menopause. However, if a period pops up in the middle of that year, the clock gets reset—till a whole year without a period goes by.
Menopause:
That year without flow dispatches you into menopause, which goes on for the rest of your life. For a general idea on when you might hit menopause, Prior observes that “The average age of menopause in Western countries is approximately 51.”
This is just a small slice of Going Menopostal. Order the book now.