Hormone health 101: Meet the 6 hormones that affect your life during menopause
You probably already know that perimenopause and menopause are all about changing hormones. But which hormones are they, what do they do – and why do they have such a major impact on your life?
First the basics: Menopause is the complete cessation of your menstrual cycle. Medically you are considered to be in menopause if you haven’t had a period for 12 continuous months. Perimenopause refers to the natural transition from your normal reproductive cycle to menopause. However, this period-free phase of life comes with its own set of health issues, which are due to the hormonal changes your body undergoes. So, here’s a breakdown of the hormones involved in this phase (estrogen, estradiol, progesterone, testosterone, cortisol, and serotonin).
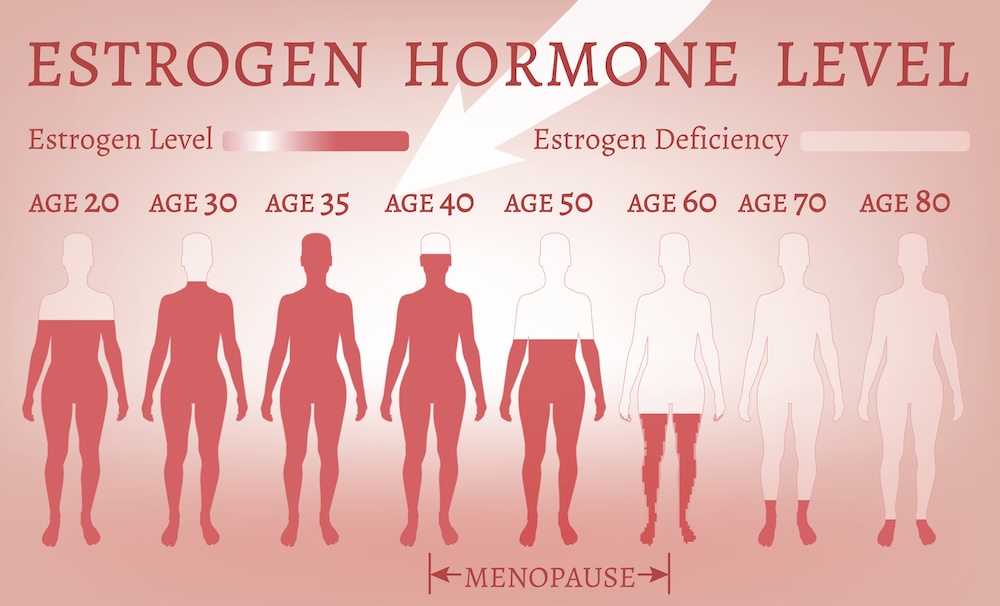
1. Estrogen
You have probably heard a lot about estrogen, but how does it affect your life? Basically, estrogen (along with progesterone) helps you to have a normal reproductive cycle. Menopause decreases your estrogen levels as the supply of mature eggs in your ovaries diminishes and you begin to produce less and less estrogen. This loss of ovarian estrogen results in the commonly seen and discussed menopausal symptoms such as hot flashes and vaginal dryness.
The loss of estrogen doesn’t affect only your reproductive system. Premenopausal women have a much lower incidence of cardiovascular disease than men, as estrogen plays a protective role. Estrogen lowers your bad cholesterol (HDL) and increases your good cholesterol (LDL) which protects you against blockage in your arteries. However, this benefit is lost once you hit menopause and studies have shown a dramatic increase in atherosclerosis (a thickening or hardening of arteries caused by a buildup of plaque in an artery’s inner lining) in postmenopausal women. The loss of estrogen has also been associated with an increase in abdominal fat – and belly fat can lead to obesity if left unchecked.
In the late 1990s, the traditional approach to falling hormonal levels in menopause was Hormone Replacement Therapy (HRT), which was prescribed to approximately 15 million women per year. Then a widely misinterpreted study called the Women’s Health Initiative turned those numbers upside down. The study was designed to look at HRT and whether it helped reduce cardiovascular risk. In 2002, it abruptly stopped due to the clinical trial linking a combination of estrogen and progestin (a synthetic form of progesterone) with an increased risk of heart disease, stroke, blood clots and breast cancer. Once the results were made public, women panicked and canceled their HRT prescriptions. This fear persisted for decades, with even physicians and government officials changing guidelines on HRT.
More recently, we have come to realize just how flawed this study was and that the way its results were presented caused women to cancel a therapy that was helping them navigate an under-researched part of life. Yes, the increased risk of breast cancer was accurate but the study also had a major design flaw: It included women in their 60s and older (who already had an increased risk of health conditions) instead of healthier women in their 50s who were also likely to have more symptoms of menopause. Another limitation stated in their paper itself was that this increased risk of cancer revolved around a specific formulation of HRT – one that is no longer in use today. And, the increased breast cancer risk only emerged with women who took hormones for over five years.
“Other formulations are currently used including estradiol, estrogen and progesterone alone as well as in combination” notes Dr. Sakeena Shaik, PharmD at theJawaharlal Nehru Technological University in India. She also says that women who are unable to use these hormone replacement therapies have other forms of hormone therapy available, such as Selective Estrogen Receptor Modulators (SERMs).
According to the Mayo Clinic, the risks of Hormone Replacement Therapy depend on the type of therapy, the duration, the dosage and your individual risk factors. Meaning, any woman considering HRT for menopausal symptoms should consult with her medical provider for personalized advice.

2. Progesterone
Progesterone is a steroid hormone that helps maintain a pregnancy. When you enter perimenopause, the levels of progesterone (along with estrogen) start to decrease. This decrease in progesterone was seen to increase uterine fibroids in the perimenopausal period.
Progesterone and reproductive hormones in general play a protective role in sleep apnea meaning many women generally have a lower incidence sleep-disordered breathing before menopause, but the reduced levels of progesterone and estrogen put menopausal women at an increased risk of obstructive sleep apnea – a condition where the muscles of your mouth can partially or completely block your airway while sleeping. (As noted above, although researchers are working on new formulations of hormone therapy that will minimize the risk of breast cancer, taking HRT with progesterone can be problematic if you have a high risk of breast cancer – so always consult your doctor before starting it.)
3.Estradiol
Estradiol is an estrogen hormone – the most powerful one. As estrogen decreases in perimenopause and menopause, so does estradiol. One of the many functions that estradiol plays is around muscle regeneration. With decreasing estradiol levels in perimenopause and menopause, your muscle health can be impacted, and you may see decreased bone strength, muscle mass and muscle strength commonly in women in perimenopause and menopause. Estradiol is also involved in the regulation of your immune systems which means that as estradiol levels fall, inflammation increases.
4. Testosterone
Testosterone is mainly a male hormone but it is also present in women – just like estrogen is present in men. Though previous studies reported inconsistencies on the level and role of testosterone, a study performed by the University of Regina in 2021 showed that the ratio of testosterone and estradiol increases as you age and get closer to menopause. An increased ratio of these two hormones has been associated with poor sleep quality, depressive symptoms, and hot flashes. Unlike estrogen, testosterone therapy has not been widely researched in menopausal women.
5. Cortisol
Cortisol is a glucocorticoid, a type of steroid hormone that is produced by adrenal glands that sit on top of your kidneys. It slows down the body’s non-essential functions in case you are in a dangerous situation. It also regulates your immune system responses, suppresses your digestive functions, and growth functions and basically works as your body’s “alarm system,” helping to regulate your body’s response to stress. Glucocorticoids also play a part in your body’s circadian rhythm and can affect sleep-wake cycles: If your cortisol is at a normal level, you have lower levels in the evening and higher ones in the morning. [Note: Optimal levels of cortisol are crucial for maintaining bodily functions; read more about cortisol and the body’s adrenal system in this previously published Midst article by Dr. Thara Vayali, ND.]
6. Serotonin
Though estrogen may seem to top the list of hormones that affect a lot of your organs, serotonin is the one that may actually be the most important. A 2018 review paper published in the Annual Review of Medicine stated that the majority of serotonin is found outside the central nervous system (brain, spinal cord) but serotonin regulates virtually all human behaviors. Some of the bodily functions affected by serotonin include mood, appetite, anger, memory, etc. The paper goes on to say that, “it is difficult to find a human behavior that is not regulated by serotonin.”
The metabolism of serotonin is controlled by estrogen. Though previous studies stated that menopause caused an increased risk of depressive disorders, a 2024 study published in The Lancet showed that other factors may be at play when it comes to depressive disorders in menopausal women.
Menopause and hormone changes
Most of the changes – if not all – in perimenopause and menopause can be tracked to increased or decreased hormone levels in your body. And, many more hormones – such as insulin – may be affected and make your symptoms worse.
Supporting your body as it goes through this hormone-depleted state is important. Ruhma Nazeer, a consultant dietician from the University of Agriculture, Faisalabad, suggests eating soybeans, chickpeas and flax seeds (to support your falling estrogen levels) and quality proteins and complex carbs (for progesterone). She also suggests trying to keep calcium, vitamin B complexes, vitamin E, and vitamin D in their optimum levels. And, since every woman can have different symptoms and hormonal levels, it’s important that healthcare providers provide a personalized approach to menopause. So, talk to your doctor for the best, most customized advice.