
I stopped breathing 16 times a night. Here’s what I did about my sleep apnea.
Perimenopause is legit, no joke. You already know this. The list of potential symptoms is seemingly endless: Hot flashes, insomnia, memory fog, heart palpitations, weight gain, bloating, bladder incontinence, a tanking libido, night sweats, random allergies, burning mouth syndrome (wtf?).
Add sleep apnea to that list. Ba-dum-tss.

What is sleep apnea exactly?
According to Mayo Clinic, there are three types of sleep apnea:
- Obstructive sleep apnea (OSA) is the most common and happens when throat muscles relax and block the airway during sleep, leading to snoring and interrupted breathing.
- Central sleep apnea (CSA) is less common. This can be induced by high altitude, heart failure, and nervous system damage, failing the brain to alert the muscles that control breathing.
- Treatment-emergent central sleep apnea, also known as complex sleep apnea, is a rare mix of OSA and CSA. A person may already have OSA but develop CSA while receiving OSA treatment.
Who knew? Until recently, I’d never heard of any women around me dealing with this condition, let alone during perimenopause and menopause.
How many women experience sleep apnea?
An estimated 30% of women over the age of 40 experience moderate or severe sleep apnea, and the chances only increase with aging, per Elektra Health. If left untreated, women can experience high blood pressure, heart attack or heart failure, strokes, and potentially Type 2 Diabetes, weight gain, anxiety, and more.
And according to research from Yale Medicine, “progesterone and estrogen may protect women against sleep apnea, but menopause cancels out that benefit. Older women are just as likely to develop sleep apnea as are men; if you have this condition, oxygen deprivation may cause you to awaken several times during the night.”
Stasia Wieber, MD, Medical Director at Northeast Medical Group Sleep Center in Fairfield, Connecticut, and a sleep disorder specialist, says she is seeing more women diagnosed with sleep apnea due to the decrease of the progesterone lining in the throat, which typically starts in perimenopause. “We know the levels of progesterone are diminished [in perimenopause and afterward], and this may cause insomnia, sleep apnea, and night sweats,” Wieber explains. “Also, an increase in BMI in peri-post menopause is also a risk factor for obstructive sleep apnea.”
Hormones are all over the place during perimenopause, and we know our sleep is all over the place because of that.
Those with sleep apnea are known for snoring loudly. Sometimes, they even stop breathing, according to whoever is sleeping beside them. My dad, who was diagnosed in the early ‘90s and the only person I ever knew with this condition, stopped breathing 85 times a night on average. Other symptoms include crankiness, headaches in the morning, a dry mouth after sleeping, grogginess during the day or hypersomnia, a lack of focus, and insomnia.
“My dad stopped breathing 85 times a night on average.”
Sleep apnea happened to me
Under Dr. Wieber, I was diagnosed with moderate obstructive sleep apnea in November 2023 (My BMI was 28.2). According to my exhausted husband, this was after countless nights of obnoxiously snoring and snorting. The snorting, especially, would wake me up from my sleep quite often. I experienced other common post-shuteye symptoms, such as dry mouth and occasionally daytime sleepiness or lack of energy.
I just thought this stuff was regular adulting — the whole work-life/home-life balancing act, y’know? I typically chalked it up to weather (it’s dryer in the winter on the East Coast) and the usual sinus infections during those colder months. This behavior was more consistent in the winter but gained momentum as I reached 45 and added an extra 10-15 pounds during the pandemic.
But at the same time, I was used to my weight yo-yo-ing since having my son in 2013. I thought, “I’m an active person. I work out consistently and maintain a healthy diet. This is all happening because I gained some weight.”
My husband was over the disruptions, and honestly, so was I. Snoring isn’t exactly sexy or becoming. But with that triviality aside, I just wanted to sleep better and didn’t want to interrupt my husband’s sleep time. Then I thought, hmm… perhaps this is genetic, or could this be related to perimenopause?

My inkling was greatly supported upon discussing this with my primary care physician, who referred me to Dr. Wieber. Within weeks, I did an at-home Respironics NightOne sleep apnea test; however, a clinical suspicion of obstructive sleep apnea was detected, and more data was required, so off to the sleep lab I went for a more comprehensive nocturnal polysomnography. I was hooked up to countless sensors, plus sticky goop, to keep them in my hair so my sleep activity and heart, brain, and respiratory system could be thoroughly tracked.
To my surprise, I slept better than I thought I would.
In the end, along with a proper diagnosis of moderate OSA, my study results indicated severe apnea in REM sleep, plus periodic limb movements and, of course, snoring. My RDI (Respiratory Disturbance Index) was 16, indicating I stopped breathing 16 times during sleep.
“Obstructive sleep apnea can range from mild to severe,” as explained by Johns Hopkins Medicine. “This is based on a measurement rating system called the apnea-hypopnea index (AHI). The AHI measures an average number of apnea and hypopnea episodes you have per hour that you sleep.”
The range for adults to be diagnosed with OSA is classified by:
- Severe obstructive sleep apnea = an AHI < 30 or 30+ episodes per hour.
- Moderate obstructive sleep apnea = an AHI between 15 and 30.
- Mild obstructive sleep apnea = an AHI between 5 and 15.
- Normal sleep means = an AHI is > 5.
I am incredibly grateful for answers, and my CPAP machine is a lifesaver — literally. I no longer stop breathing while slumbering. Everyone, including my dog Winston, is snoozing better than ever! Another bonus: the CPAP machine counts as a free carry-on when traveling.

I do wake up occasionally if my mask is off-center. This can make a slight hissing noise, which is quite annoying. Aside from that, sleep apnea is manageable. Keeping my device clean is simple, and having distilled water is a must for your humidifier.
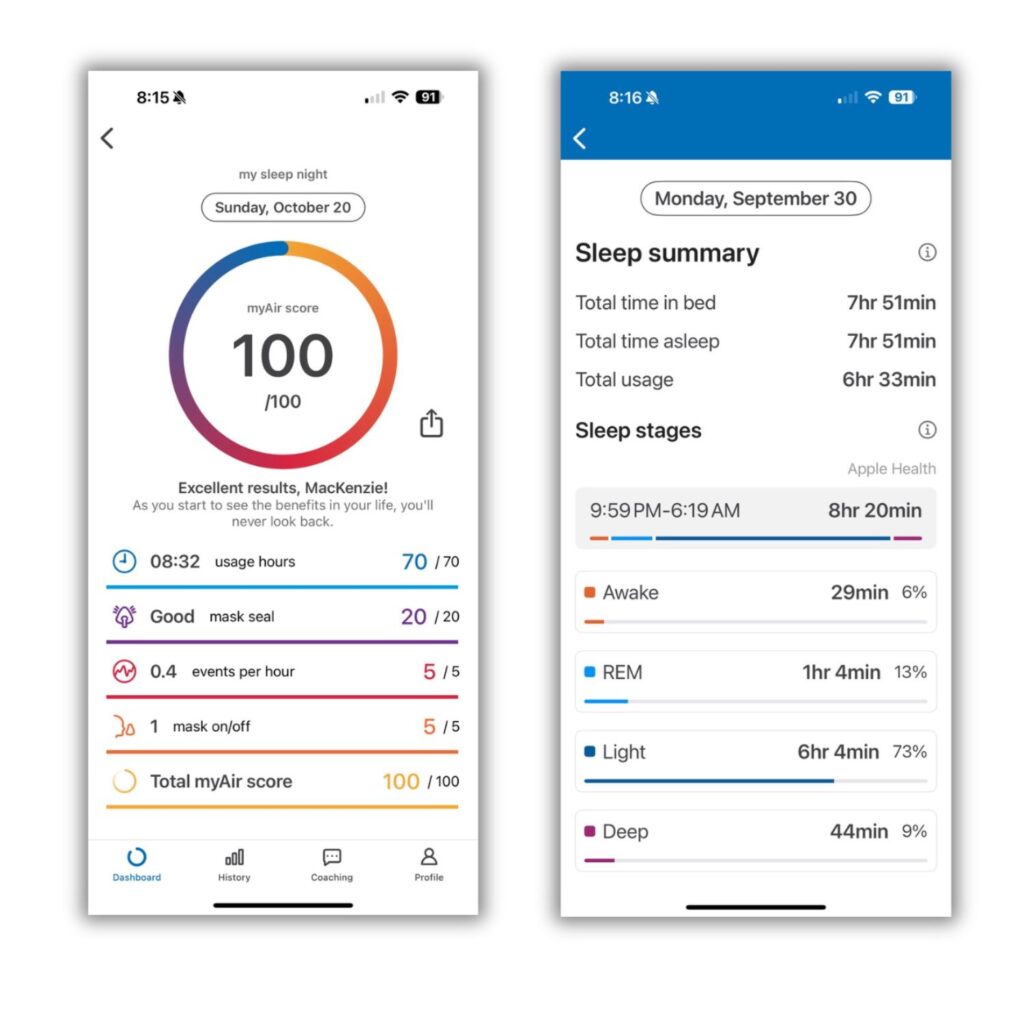
My CPAP Machine works brilliantly with the myAir app, which tracks my daily machine usage, mask seal, any events per hour, and if my mask is off. Plus, the sleep summary is super helpful for comparing various sleep stage data and then some!
Knowledge is power! Contact your doctor if you suspect you are experiencing Sleep Apnea symptoms. Or, if you are already using your CPAP machine, high fives! Yale also suggests adding “soy-rich foods, which are high in phytoestrogen (a chemical that mimics the effect of estrogen in your body), into your diet.”
New to perimenopause? We got you. Start here.



