Chronic pain is rising among women. Why are autoimmune disorders such a little-known culprit?
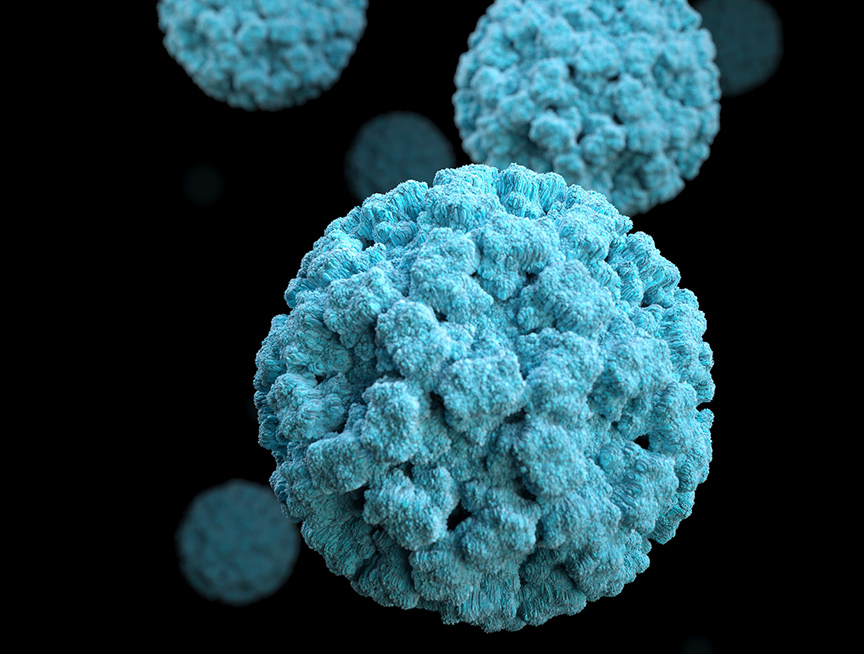
Autoimmune diseases (ADs) are a group of disorders that have one maddening aspect in common: sufferers’ immune systems malfunction and attacks healthy parts of their body. Basically, the very same system that keeps you alive every day by protecting you from pathogens, hidden toxins, and homegrown threats that could turn into cancer…turns on you.
In some cases, a specific organ or tissue type is targeted. Examples in this category include Multiple Sclerosis and Hashimoto’s disease. Other times, the immune attack is more generalized, causing systemic disorders like Rheumatoid Arthritis and Lupus.
These are just a few examples of the more than 80 types of autoimmune diseases. While gender risk varies by type, women make up an overwhelming 80% of total cases. There are no known cures. ADs as a group are among the top 10 causes of death for females in the United States.
Like other “women’s diseases,” there’s a longstanding history of neglect, in terms of research funding as well as skepticism within the medical system. Women in pain are more likely to be dismissed as “chronic complainers,” or hormonal hypochondriacs. And for Black women, persistent racist myths and biases are associated with systematic undertreatment of their chronic pain.
Autoimmune disease cases are rising
Currently, ADs affect more than 24 million people in the United States, but the truth is, no one knows the exact number because there’s no official “tracking system,” though that’s beginning to change. The non-profits Autoimmune Registry and Autoimmune Research Network have started much-needed patient databases for research and statistics. Going forward, a more precise picture should come into focus, but in the meantime, the trendline is clear — cases of AD are increasing. This is very concerning, because the impacts that these kinds of illnesses have on people are profound.
Many people who have autoimmune disorders suffer from these common symptoms:
- Joint pain and swelling
- Fatigue
- Skin rashes
- Swollen glands
- Fevers
- Digestive problems
It’s like having the flu … but with ADs, you’re not better after a few days. According to the Centers for Disease Control and Prevention, rheumatic ADs are one of the leading causes of disability in adults under 65.
Beyond quality of life, “almost all ADs decrease life expectancy,” said Dr. Betty Diamond, a prominent autoimmune researcher, in an interview for U.S. News and World Report. While many ADs don’t directly shorten life span, especially with treatment, there’s a growing list of diseases that many ADs are linked to, including the two most common causes of death: cardiovascular disease and cancer.
On a larger level, there’s the daunting challenge of providing equitable access to the limited number of specialists and growing number of expensive treatments that many ADs require.
Researchers are concerned that this rising incidence in AD is real and not completely due to more diagnosed cases. The most common biomarker for autoimmunity — Antinuclear Antibodies, or ANA — has been increasing in the general U.S. population over the past 25 years. So what gives?
Nature vs. nurture or a bit of both?
In the age of genomics, the inherited side of the nature vs. nurture equation has become easier to explore. Researchers estimate that about 30% of AD risk can be attributed to an individual’s genetics. But there isn’t a single “autoimmune gene.” The human genome contains many genes that influence an individual’s risk; some people have a genetic profile that predisposes them to developing AD.
Trying to figure out what’s contributing to the other 70% of AD risk — on the nurture side — is a lot trickier. The problem is that research on how environmental exposures might trigger AD in susceptible people is generally limited to observational studies. So it can be difficult to prove anything beyond mere association. For example, by studying questionnaires of sleep habits and health history, researchers have found a link between not getting enough sleep and the risk for developing Lupus. But because other possible factors that might also explain this connection aren’t controlled for in this type of study, it’s not possible to prove anything beyond mere association.
The list of environmental exposures associated with AD is long, varied, and growing. But if we simply look at a worldwide map of where ADs are increasing, we see an overlap with adoption of a Westernized, or standard American diet. We all know what that is: Big Mac, Filet-o-fish, Quarter Pounder, French fries, icy Coke, thick shake, sundae, and apple pie. Or, simply most of the foods in our grocery stores or on restaurant menus.
Food matters so much because there’s growing evidence pointing to how changes in the microbes and lining of the gut contribute to AD development. As the world-renowned gastroenterologist and autoimmune researcher Dr. Alessio Fassano wrote almost a decade ago, “The gut is not like Las Vegas: What happens in the gut doesn’t stay in the gut.”
Why getting diagnosed for autoimmune disease is so damn hard
In some ways, AD can seem like anything and everything.
The list of possible factors contributing to AD continues to grow and might seem like almost anything can be a trigger. From natural infections to synthetic plastics. From outdoor air pollution to indoor secondhand smoke. From additives in processed foods to forever chemicals in beauty products.
The number of symptoms can also be confusing. Everything that hurts might be a symptom of an AD. Some symptoms are rather mild and common. Fatigue, achy joints, headaches, bloating. Others would keep you in bed all day or send you to the ER.
Everything that hurts might be a symptom of an AD. Some symptoms are rather mild and common. Fatigue, achy joints, headaches, bloating. Others would keep you in bed all day or send you to the ER.
Finally, the course of AD can be just as baffling. For some, symptoms remain mild or the AD may even go into remission, where it seems to disappear. For others, flares lead to rapid progression. And it’s not always clear which pathway someone will take. On top of that, many ADs have mixed and overlapping symptoms that unfold gradually over time. One in four people with AD will eventually develop more than one type.
This ambiguity makes getting diagnosed frustratingly difficult for many. There isn’t an “autoimmune doctor” or a simple test that can quickly tell you if you have an AD. On average, it takes patients four years and four doctors to get a diagnosis.
Now time for the good news. Over the past few decades, so much has been learned about ADs, from genetics to pathology to diagnostics. Advances in biotechnology have expanded drug therapy options. The National Institute of Health (NIH) has recently committed to “amping up” investments in AD research and may even be creating a new Office solely focused on ADs.
We’re even beginning to develop answers to the many “why?” questions that have long been asked. Let’s start with the most obvious one.
Why are women more vulnerable to autoimmune disease than men?
Estrogen has long been the primary explainer of differences in gender risk. This makes sense because many ADs have an onset after puberty but before menopause. In addition, ADs are often triggered during times of hormonal shifting, such as in the postpartum or perimenopausal period.
Recently, scientists are finding explanations at an even more basic level of biology. They now think that much of the answer boils down to whether you have two X chromosomes (i.e., people typically identified as female) making up your 23rd pair, versus only one X and one Y chromosome, (i.e., people identified as male). as those who are born male have
It turns out that the 23rd X chromosome is loaded with many immune-regulating genes. So if you have two of them — great! — you may have a stronger immune system. This may explain why women are less vulnerable to dying from infections like COVID-19 and even why women have longer lifespans.
But the second X chromosome itself can become a problem if it’s recognized as foreign by parts of your immune system. During female fetal development, each cell inactivates, or silences, one of the X chromosomes. If this random process is skewed heavily to one lineage, autoimmune issues may arise.
Another possible mechanism for autoimmunity is if X-inactivation is incomplete or the silenced X-chromosome becomes reactivated later in life, leading to two X chromosomes trying to control expression within the same cell. It’s like your two genetic lineages are fighting to determine which version of yourself you should be. The resulting expression of too many immune genes might lead to autoimmunity too.
Immune system 101
To understand AD, let’s look at the basics of the immune system, where AD originates. Maybe you remember learning about the immune system in high school Bio class. More recently, in the Covid-era, you’ve definitely heard terms like antibodies and immunity, probably way more than you’ve ever wanted to.
There are two basic parts to the immune system: innate and adaptive.
From birth, our innate immune system is the body’s first line of defense. This rapid response is provided through physical and chemical barriers, fevers, and immune cells that non-specifically attack invaders, such as macrophages (remember the cartoon drawings of those big, blobby white blood cells gobbling up invading bacteria?). Abnormalities can occur in the innate immune response, but problems with the adaptive immune response seem to play a more direct role in AD development.
Throughout life, our adaptive (or acquired) immune system is developing targeted immune responses to specific threats we encounter. This response is produced by two types of lymphocytes (forms of white blood cells):
- T-cells: produced in the thymus (also called “cellular” immunity)
- B-cells: produced in the bone marrow (also called “humoral” immunity)
T-cells are most active in our tissues, targeting cells that are infected or cancerous. There are three main types with specialized roles:
- Cytotoxic (or killer) T Cells destroy abnormal cells.
- Helper T Cells activate B cells and produce cytokines (proteins that regulate inflammation).
- Regulatory T Cells help keep the immune response in check.
B-cells target threats floating around in the body. They bind foreign substances (also called antigens) and then morph into plasma cells that produce antibodies specific to the antigen that the parent cell combined with. Some B-cells turn into memory cells that can produce antibodies specific to that same antigen at a future time if activated.
How does your body attack itself?
Both types of lymphocytes work in tandem and can even provide checks and balances on each other, ensuring that only dangerous pathogens or abnormally growing cells are targeted. Most of the time, our immune system works pretty well, but AD may occur when something goes wrong with either response. Sometimes lymphocytes mistakenly attack healthy cells, tissues or organs. Other times there’s a mix-up with antibodies that were produced to fight a pathogen, but are able to cross-react with healthy parts of the body.
An abnormal immune response alone does not necessarily result in AD. For example, many “healthy” people have autoantibodies (antibodies that target healthy cells), but most people never develop AD. We know that abnormal immune responses begin years before symptoms of AD show up. This could be a window of opportunity for preventing AD from the get-go.
Why is midlife a prime time for autoimmune diseases in women?
Some AD are more likely to show up before age 40, like Lupus or Crohn’s disease. Type 1 Diabetes most commonly presents in childhood. Midlife, however, remains a common age of diagnosis.
First, the time span between onset of symptoms and obtaining a formal diagnosis may be years, so even if your disease began in your 30s you might not know it until your 40s.
Second, some of the most common ADs — such as Hashimoto’s Disease and Rheumatoid Arthritis — peak during midlife.
But midlife itself might be a contributing factor too. Being middle-aged presents a perfect storm for AD to develop. An increase in inflammation. Hormonal shifting. Metabolic aging. Being old enough to accumulate a significant amount of triggering exposures, but young enough to still have a strong immune response.
In addition, mental health issues often intersect with both midlife and AD. Recent research is finding that stress and trauma raise the risk for triggering AD, whether it be something you’re currently struggling with or something you experienced years earlier.
Growing up in a culture with messages about keeping quiet can lead to holding onto pain for many years. “If you don’t have anything nice to say, don’t say anything at all.” “Put up or shut up.” And for people in marginalized groups, the silencing messages are often much stronger and more overt.
You might feel betrayal within yourself for not saying the words that needed to be said. Or maybe you feel betrayed by people you loved, or even the society at large, for not providing the space to say them, or sometimes to even breathe.
Your exposome, your future
As women look back at their lives, they see their exposome, a lifetime of social, dietary, chemical, environmental, and infectious exposures that greatly influence present and future health. Many of the environmental triggers of AD have already accumulated by midlife, many without consent, or choice.
Looking forward from the point of midlife can also be a mixed bag, especially in times of tremendous uncertainty. Lack of defined retirement benefits. Increasing costs of almost everything. Complicated relationships. Too many decisions. And nearly everyone is one medical crisis away from bankruptcy.
But somehow, in the midst of all of that, there’s a sweetness in growing older too. Taking ownership of yourself. A desire to heal past wounds, to be stronger and deeper and to forge ahead, clear-eyed about future challenges.
Though our modern diet and exposure to chronic stress and toxins won’t cause everyone to develop AD, we know they’re causing many of us to get sick and feel unwell. ADs might be a warning for all of us: we need to change how we’re living and taking care of ourselves.
Now let’s get started.
Stay tuned. We’ve got more articles about ADs in the works, including personal health stories and a look into whether there’s anything we can do now to lower our risks for developing AD.
We’re in this together! Sign up for our newsletter to stay in the loop.
We did a ton of research. Here are our sources:
Ahn JY & Lee JT. (2008) X Chromosome: X Inactivation
Arango M, et al.(2013) Infection and autoimmune diseases. In Anaya J, et al., editors. Autoimmunity: From Bench to Bedside
Armitage M. (2021). Symptom Management vs. Disease-Modifying Therapies: How to Find the Right Autoimmune Therapy For You
Autoimmune Association. (n.d.) Autoimmune Disease List
Autoimmune Association. (n.d.) Autoimmune Research Network – ARNet
Autoimmune Association. (n.d.) What is autoimmunity?
Autoimmune Institute. (2022) Symptoms & Signs of Autoimmune Disease
Autoimmune Registry. (n.d.) List of Autoimmune Diseases
Bryant E. (2021) Parents smoking during childhood linked to rheumatoid arthritis later in life
Center for Disease Control and Prevention. (2021) Arthritis Related Disabilities and Limitations
Choi MY, et al. (2022) Association of Sleep Deprivation and the Risk of Developing Systemic Lupus Erythematosus Among Women
Cojocaru M, et al. (2010) Multiple autoimmune syndrome
Criswell LA. (2022) Amping Up Our Investment in Autoimmune Disease Research
Delves PJ. (2022) Acquired Immunity
Desai MK & Diaz Brinton R. (2019). Autoimmune Disease in Women: Endocrine Transition and Risk Across Lifespan.
Dinse GE, et al. (2020). Increasing Prevalence of Antinuclear Antibodies in the United States.
Eustice C. (2022). Cytokines and How They Work.
Fasano A.. (2014). Gluten Freedom: The Nation’s Leading Expert Offers the Essential Guide to a Healthy, Gluten-Free Lifestyle.
Gianicolo EAL, et al.(2020). Methods for Evaluating Causality in Observational Studies.
He M, et al. (2021). Immune-mediated Diseases Associated with Cancer Risks.
Ho JQ, et al. (2022). The immune response to COVID-19: Does sex matter?
Hoffman KM, et al. (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites
Institute for Quality and Efficiency in Health Care. (2020) How does the immune system work?
Institute for Quality and Efficiency in Health Care. (2020). The innate and adaptive immune systems
John Hopkins Environmental Health & Engineering. (n.d.). The Expososme Collaborative Background
John Hopkins Medicine, Department of Pathology. (2022). Autoimmunity Basics: Disease Development
John Hopkins Medicine, Department of Pathology. (2022). Autoimmunity Basics: Types of Damage
John Hopkins Medicine, Department of Pathology. (2022) Definition of Autoimmunity and Autoimmune Disease
Klein SL & Flanagan KL. (2016). Sex differences in immune responses
LaMorte WW. (2019). Association versus Causation
Makin S. (2021). Cracking the genetic code of autoimmune disease
Mayo Clinic. (2022). Crohn’s disease
Mayo Clinic. (2022). Type 1 Diabetes
Mayo Clinic Staff. (2022). What is Multiple Sclerosis? An expert explains
Mazzucca CB, et al. (2021). How to Tackle the Relationship between Autoimmune Diseases and Diet: Well Begun is Half-Done
McCarthy M & Raval AP. (2020). The peri-menopause in a woman’s life: a systemic inflammatory phase that enables later neurodegenerative disease
Mirin AA. (2021). Gender Disparity in the Funding of Diseases by the U.S. National Institutes of Health.
Mishra A, et al. (2022). A tale of two systems: Lessons learned from female mid-life aging with implications for Alzheimer’s prevention & treatment.
Moore A. (2020). Immunosuppressive Meds for the Treatment of Autoimmune Disease.
Moulton VR. (2018). (Sex Hormones in Acquired Immunity and Autoimmune Disease.
National Academies Press. (2022). Enhancing NIH Research on Autoimmune Disease.
National Cancer Institute. (n.d.). Antibody.
National Cancer Institute. Antigen. (n.d.). Antigen
National Institute of Allergy and Infectious Diseases. (2014). Features of an Immune Response.
National Institute of Environmental Health Sciences. (2022). Autoimmune Diseases.
National Institutes of Health. https://www.nih.gov/
National Pharmaceutical Council. (2022). Addressing the Needs of People Living with Autoimmune Disorders: A Conversation with Molly Murray.
Nowak K, et al.(2019). Immunomodulatory effects of synthetic endocrine disrupting chemicals on the development and functions of human immune cells.
Orbai A. (n.d.). What Are Common Symptoms of Autoimmune Disease?
Partridge D, et al. (2019). Food additives: Assessing the impact of exposures to permitted emulsifiers on bowel and metabolic health – introducing the FADiets study
Roberts AL, et al. (2017). Association of Trauma and Posttraumatic Stress Disorder With Incident Systemic Lupus Erythematosus in a Longitudinal Cohort of Women
Samulowitz A, et al. (2018). “Brave Men” and “Emotional Women”: A Theory Guided Literature Review on Gender Bias in Health Care and Gendered Norms towards Patients with Chronic Pain
Song H, et al. (2018). Associations of Stress-Related Disorders With Subsequent Autoimmune Disease
US Department of Health & Human Services, Office on Women’s Health. (2021). Autoimmune diseases
Wenger NK.(2019). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6671777/
Whitehead HD, et al. (2021). Fluorinated Compounds in North American Cosmetics
Vojdani A, et al. (2014). Environmental Triggers and Autoimmunity
Vojdani A, et al. (2022). The Role of Exposomes in the Pathophysiology of Autoimmune Diseases II: Pathogens
Yale School of Medicine. (2020). Untangling the Web of Autoimmune Diseases
Yuen GJ. (2020). Autoimmunity in Women: an eXamination of eXisting models
Zhao N, et al. (2022). Long-term exposure to fine particulate matter and ozone and the onset of systemic autoimmune rheumatic diseases: an open cohort study in Quebec, Canada